In vitro fertilization (IVF) is a cornerstone of the surrogacy process. It is the method through which an embryo is created outside the body before being implanted in the surrogate’s uterus. IVF makes it possible for intended parents to have a biological child through a surrogate, even if they are unable to carry a pregnancy themselves. Understanding the role of IVF in surrogacy is essential for intended parents, as it will help them navigate medical, emotional, and financial aspects of the journey.
This guide explains the IVF process as it relates to surrogacy, covering key stages, what to expect, and the critical decisions that need to be made.
1. The Basics of IVF in Surrogacy
In surrogacy, IVF plays a crucial role in creating the embryos that will be implanted in the surrogate. IVF allows for the fertilization of eggs outside the womb, which is essential when the intended mother is unable to carry a pregnancy, or when there is an issue with the intended mother’s uterus, eggs, or other fertility factors.
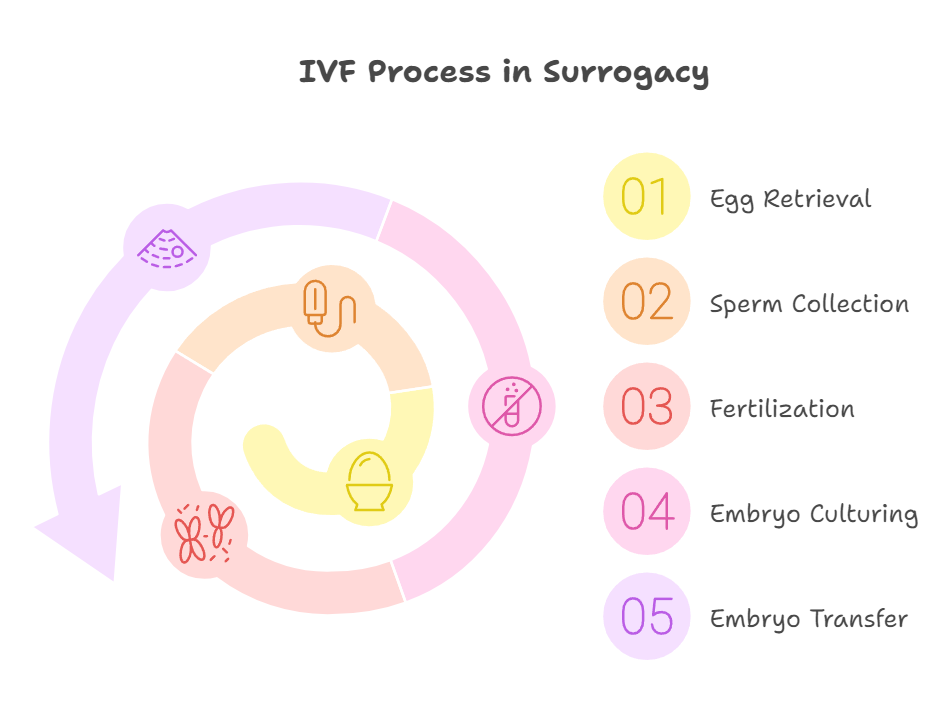
The IVF process for surrogacy involves several key steps:
- Egg Retrieval (Oocyte Retrieval): The intended mother’s or an egg donor’s ovaries are stimulated with hormones to produce multiple eggs. Once the eggs are mature, they are retrieved through a minor surgical procedure.
- Sperm Collection: The intended father or sperm donor provides sperm, which is used to fertilize the eggs.
- Fertilization: The sperm is used to fertilize the eggs in a lab, creating embryos. In some cases, Intracytoplasmic Sperm Injection (ICSI) is used, where a single sperm is injected directly into an egg to ensure fertilization.
- Embryo Culturing: The fertilized embryos are cultured in the lab for several days (typically 3 to 5), allowing doctors to monitor their development.
- Embryo Transfer: Once viable embryos are ready, one or more are selected for transfer into the surrogate’s uterus. This is a simple, non-invasive procedure that doesn’t require anesthesia.
What to Consider:
- IVF is the primary method for creating embryos in surrogacy, but the specifics of the process may vary depending on the medical history of the intended parents and the surrogate.
- There may be multiple embryo transfers before a successful pregnancy, depending on the quality of the embryos and the response of the surrogate’s uterus.
2. Genetic Material and Donor Options
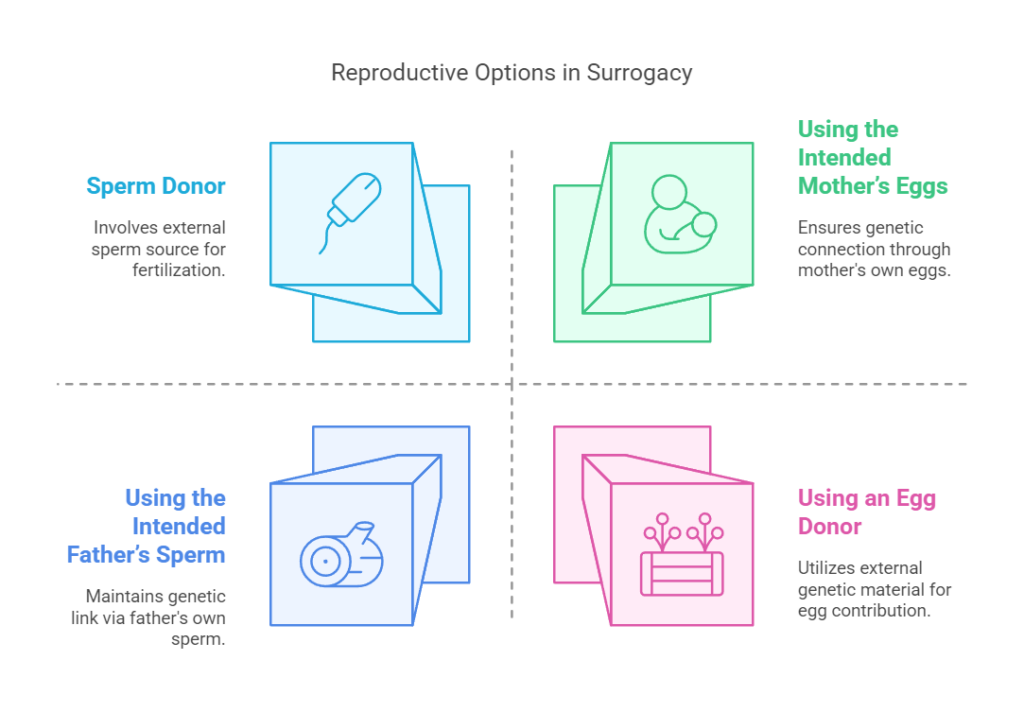
In surrogacy, one of the most significant decisions involves the source of the genetic material—specifically the eggs and sperm used to create the embryos.
What to Consider:
- Using the Intended Mother’s Eggs: If the intended mother is producing healthy eggs, she can provide her own eggs for IVF. This allows the child to be genetically related to the intended mother.
- Using an Egg Donor: If the intended mother is unable to produce viable eggs, or if there are genetic concerns, egg donation may be an option. This means the eggs will come from a separate woman, and the intended mother will not have a genetic link to the child.
- Using the Intended Father’s Sperm: Typically, the intended father’s sperm is used, though sperm donation is also an option if the father has fertility issues or genetic concerns.
- Sperm Donor: If the intended father cannot produce viable sperm, or if using a known sperm donor is preferred, sperm from a donor may be used.
What to Consider:
- When using egg or sperm donors, intended parents should work with a reputable fertility clinic to ensure donor anonymity, legal considerations, and medical history are clear.
- The decision about genetic material should be made in consultation with fertility specialists and may involve genetic counseling.
3. Embryo Screening and Genetic Testing
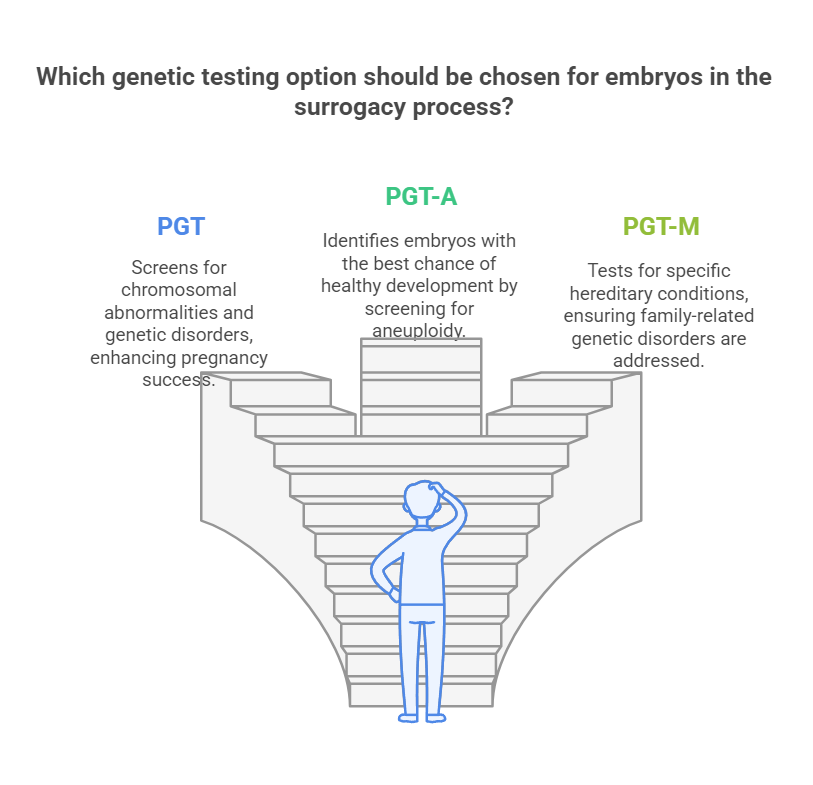
One of the advantages of IVF in surrogacy is the ability to perform genetic screening and testing on the embryos before they are implanted. This step can reduce the risk of genetic disorders and improve the chances of a successful pregnancy.
What to Consider:
- Preimplantation Genetic Testing (PGT): PGT allows doctors to screen embryos for chromosomal abnormalities or genetic disorders, such as Down syndrome, cystic fibrosis, or other hereditary conditions.
- PGT-A (Preimplantation Genetic Testing for Aneuploidy): PGT-A screens embryos for chromosomal abnormalities, helping identify the embryos with the best chance of implanting and developing into a healthy pregnancy.
- PGT-M (Preimplantation Genetic Testing for Monogenic Disorders): PGT-M is used to test for specific genetic conditions that run in the family.
- Embryo Selection: After genetic testing, the healthiest embryos are selected for transfer, increasing the likelihood of a successful pregnancy and birth.
What to Consider:
- Genetic testing can add additional costs to the surrogacy process but may increase the chances of a healthy pregnancy and reduce the risk of miscarriage.
- The decision to undergo genetic testing is personal and should be discussed with fertility specialists and genetic counselors.
4. IVF and Surrogate Health
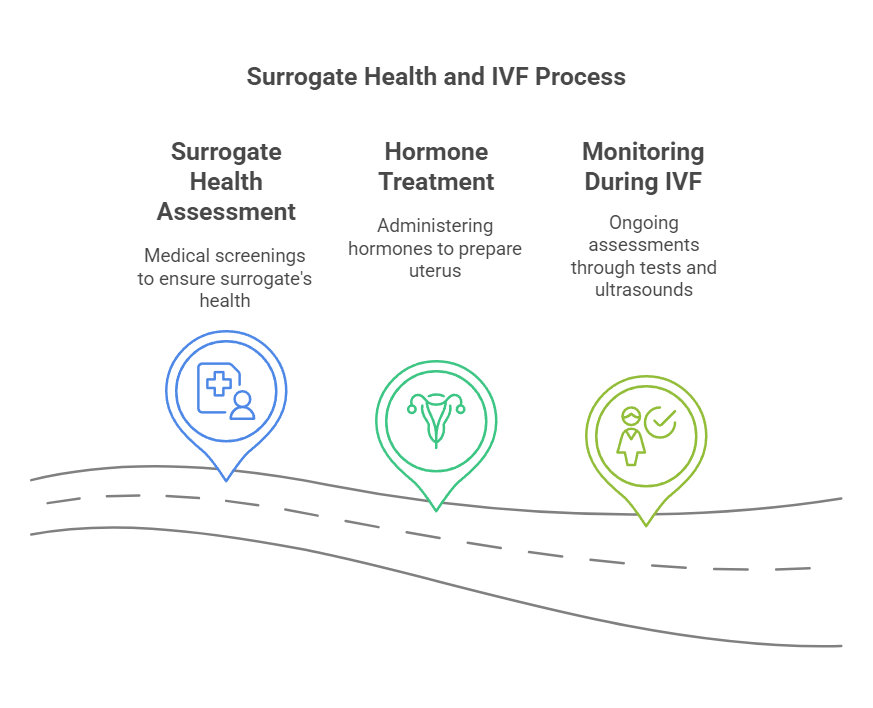
For a successful surrogacy journey, the health of the surrogate is just as important as the health of the embryos. IVF requires careful coordination between the intended parents, fertility clinic, and surrogate.
What to Expect:
- Surrogate Health Assessment: Before IVF begins, the surrogate undergoes medical screenings to ensure she is healthy and capable of carrying a pregnancy. This includes blood tests, an ultrasound of the uterus, and a psychological evaluation.
- Hormone Treatment: In order to prepare her body for embryo implantation, the surrogate typically undergoes hormone treatments (e.g., estrogen and progesterone) to synchronize her cycle and prepare the uterus for pregnancy.
- Monitoring During IVF: Throughout the IVF process, the surrogate will undergo monitoring through blood tests and ultrasounds to assess her response to the medications and the state of her uterus.
What to Consider:
- The surrogate’s health and readiness are critical for the success of the IVF and pregnancy. It’s essential to work closely with the fertility clinic to ensure the surrogate is receiving the appropriate care.
- The intended parents should maintain open communication with the surrogate to ensure she is comfortable and well-supported during the process.
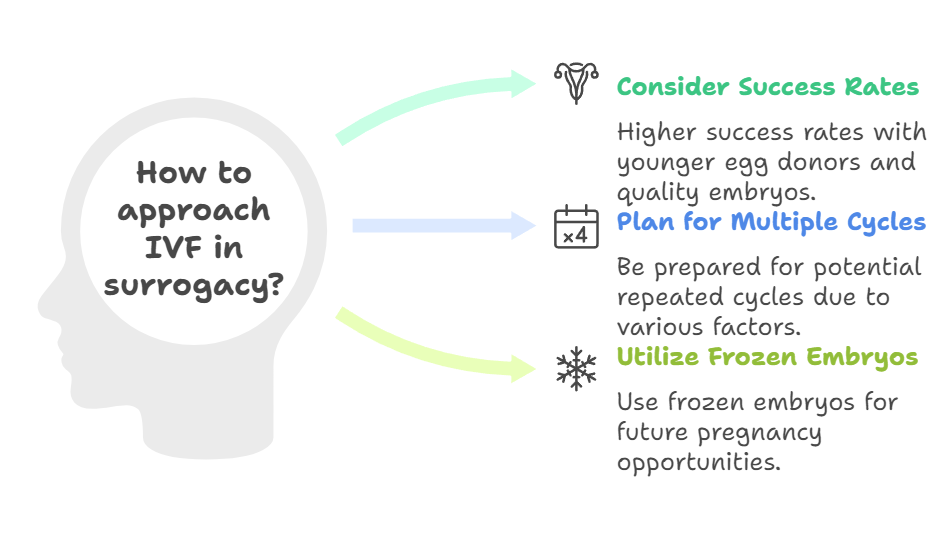
5. Success Rates and Multiple Cycles
IVF success rates can vary based on factors like the quality of the embryos, the age of the egg provider, the health of the surrogate, and the clinic’s success rate. It’s important for intended parents to understand that multiple IVF cycles may be necessary to achieve a successful pregnancy.
What to Expect:
- Success Rates: IVF success rates generally depend on the age of the egg provider and the quality of the embryos. Younger egg donors tend to produce higher-quality eggs, which can increase the chances of a successful pregnancy.
- Multiple Cycles: In some cases, it may take more than one IVF cycle to achieve a pregnancy. This could be due to factors such as embryo quality, the surrogate’s uterine environment, or other medical considerations.
- Frozen Embryos: If extra embryos are created during the IVF process, they may be frozen for future use. This provides additional opportunities for pregnancy without requiring another full IVF cycle.
What to Consider:
- Be mentally and financially prepared for the possibility of needing multiple IVF attempts. While success is possible on the first try, many intended parents go through several cycles before achieving pregnancy.
- Research your fertility clinic’s success rates and ask questions about their approach to IVF in surrogacy.
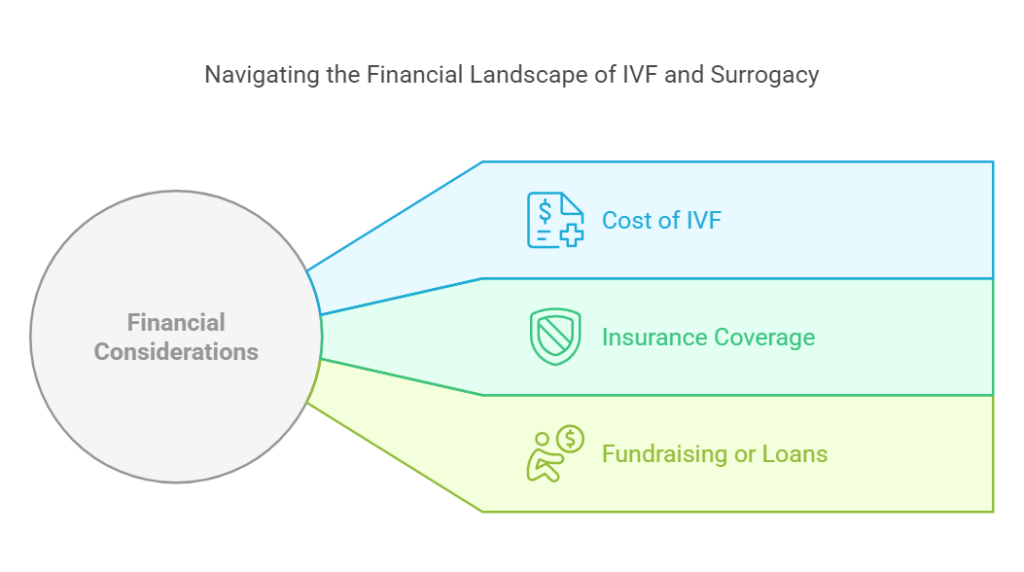
6. Financial Considerations
IVF is a significant financial investment in surrogacy. The costs associated with IVF can add up quickly, especially when considering the need for multiple cycles, genetic testing, medication, and surrogate medical care.
What to Consider:
- Cost of IVF: The cost of IVF itself can range from $10,000 to $20,000 per cycle, and this doesn’t include the cost of the surrogate’s medical care, legal fees, or other surrogacy-related expenses.
- Insurance Coverage: Some insurance plans cover part or all of the IVF process, though this is rare in surrogacy arrangements. Be sure to check with the fertility clinic and insurance provider about what is covered.
- Fundraising or Loans: Many intended parents explore fundraising options, loans, or financial assistance programs to help cover the costs of IVF and surrogacy.
What to Consider:
- Make sure to include IVF costs in your overall surrogacy budget. Consulting with a financial advisor or surrogacy agency can help you plan effectively.
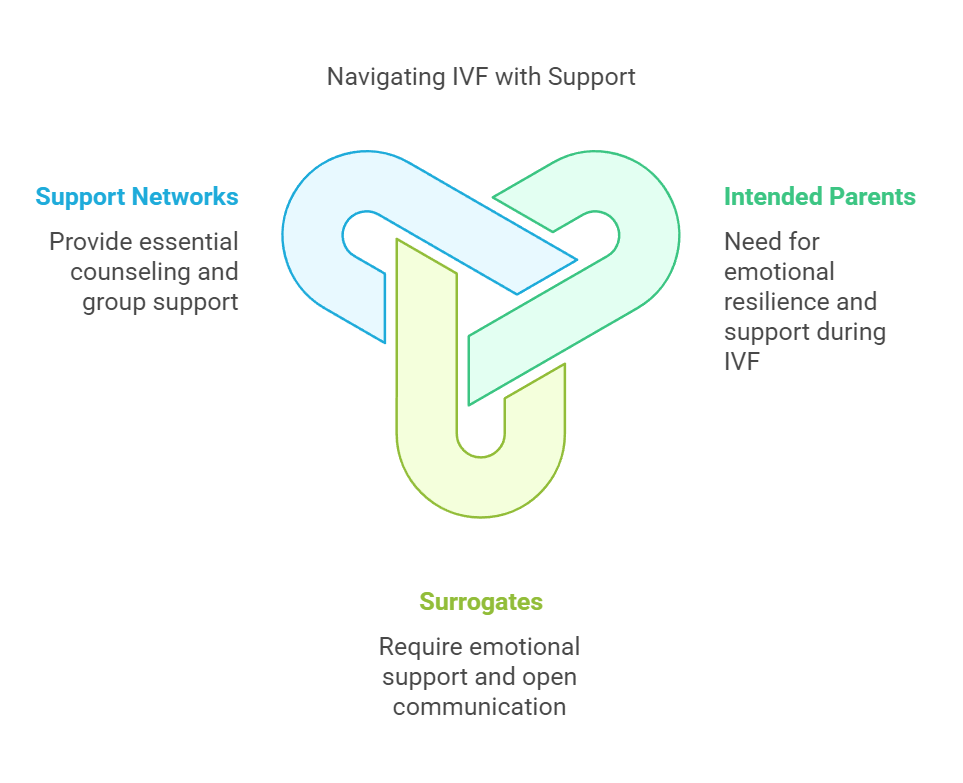
7. Emotional Considerations During IVF
The IVF process can be emotionally taxing for both the intended parents and the surrogate. The hope, anticipation, and anxiety associated with IVF cycles can make this stage of the surrogacy journey particularly intense. Preparing for Parenthood: Practical Tips for Intended Parents in the Surrogacy Process
What to Consider:
- Emotional Support: It’s important for intended parents to seek emotional support during IVF, whether through counseling, support groups, or leaning on close friends and family. This can help manage stress and expectations.
- Surrogate Support: Likewise, the surrogate should have access to emotional support during IVF and the subsequent pregnancy. IVF can be an emotional experience, and the intended parents and surrogate should maintain open communication and understanding.
What to Consider:
- Understand that IVF can be a rollercoaster, with high hopes followed by disappointments. Stay connected with your support network and keep a positive outlook as you navigate each cycle.
Conclusion
IVF is the heart of the surrogacy process, making it possible for intended parents to have a biological child through a surrogate. Understanding the IVF process and its role in surrogacy helps intended parents manage their expectations and navigate medical, emotional, and financial aspects of the journey. Whether it’s choosing genetic material, undergoing embryo screening, or preparing for multiple IVF cycles, being informed and prepared can help ensure a smoother, more successful path to parenthood.




